VACEP EBM Series: Acetazolamide in Acute Decompensated Heart Failure with Volume Overload
VACEP’s Evidence-Based Medicine Review Series
for Emergency Physicians
Authors: AJ Parker, MD with Paul E. Stromberg, MD, Department of Emergency Medicine at Carilion Clinic & Virginia Tech Carilion Emergency Medicine residency
Reviewer: Joshua Easter, MD, MSc (UVA Health)
Article: Acetazolamide in Acute Decompensated Heart Failure with Volume Overload
Authors: Wilfried Mullens, M.D., Ph.D., et al
Read the full study in the New England Journal of Medicine
About the EBM Review Series
VACEP’s Evidence-Based Medicine Review Series is a monthly literature review started by the University of Virginia’s Josh Easter, MD, MSc, a VACEP board member working to connect the academic community in Virginia. Physicians and residents submit their review of a recent journal article, and their summary is reviewed by emergency physician peers and published here. We invite each residency in Virginia (and D.C.) to create a faculty/resident team to submit and review articles. Email VACEP communications director Jeff Kelley to take the next step.
Goals
Provide a brief monthly synopsis of a high yield article germane to the practice of emergency medicine for distribution to all VACEP members
Provide an opportunity for a peer reviewed publication and invited presentation for faculty and trainees
Foster an academic community focused on evidenced based medicine for emergency medicine residency programs in the region
CASE
A 55-year-old man presents to your emergency department with shortness of breath and leg swelling. He reports that his symptoms have progressively worsened over the last 2 weeks. He takes 20mg of Furosemide twice daily, although he reports intermittent non-compliance due to urinary frequency. He denies chest pain, cough, or fever.
Past medical history includes heart failure with reduced ejection fraction of 40% and hypertension. Current vitals: HR 106, BP 152/88, RR 24, and an oxygen saturation of 90% on room air. Base weight is 92 kilograms, and today he weighs 96 kilograms. Physical examination reveals a S3 murmur, crackles in the bilateral lower lung fields, and 1+ pitting edema in the bilateral lower legs.
Your nurse asks if you have any orders for this patient.
About the Guidelines
Heart failure is a pervasive disease process with an incidence of 10 per 1,000 in patients over the age of 65. HF results in 1.2 million hospitalizations annually (Heidenreich, 2013; Agarwal, 2021). The 2022 Guidelines for Management of Heart Failure recommend Guideline-directed medical therapy Therapy (GDMT) for patients diagnosed with Heart Failure with Reduced Ejection Fraction (HFrEF) (Heidenreich, 2022).
These guidelines include a Class 1 recommendation and Level of Evidence B for the use of diuretic therapy in heart failure, both chronically and acutely.
Diuresis with intravenous loop diuretics remains the mainstay of treatment for acute decompensated heart failure, but the role of other diuretics during acute exacerbation is not well understood (Ellison, 2017; McDonagh, 2021).
The 2022 Guidelines also recommend a thiazide diuretic in addition to loop diuretics in patients “who do not respond to moderate or high dose loop diuretics to minimize electrolyte abnormalities” (Heidenreich, 2022). Mineralocorticoid receptor antagonists, such as spironolactone, have been shown to reduce all-cause mortality and morbidity in patients with HFrEF (Heidenreich, 2022; Pitt, 1999; Zannad, 2011).
Acetazolamide is a carbonic anhydrase inhibitor that reduces sodium reabsorption in the proximal tubule of the nephron. As of 2023, Acetazolamide has FDA approval for use in glaucoma, altitude sickness, and heart failure. Research on acetazolamide’s effect on morbidity and mortality when used as an adjunct therapy to loop diuretics in acute decompensated heart failure is lacking (Kassamli, 2011).
the Acetazolamide study
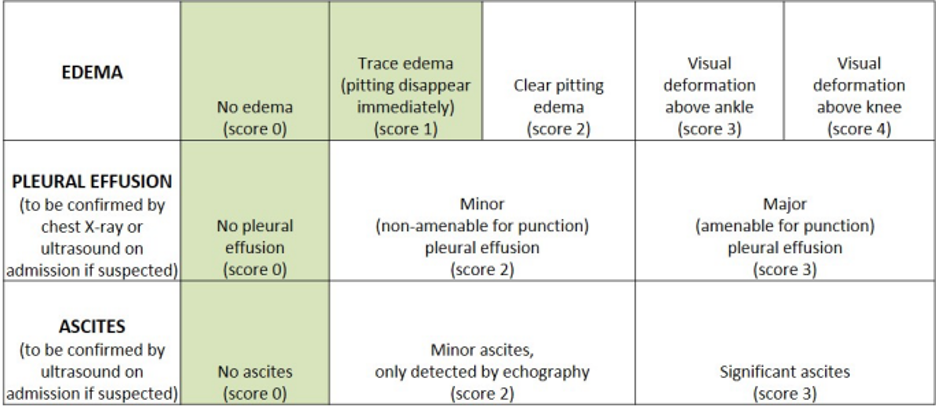
A 2022 study published in the New England Journal of Medicine, “Acetazolamide in Acute Decompensated Heart Failure with Volume Overload (ADVOR Trial),” investigated whether the addition of acetazolamide to standard diuresis improved decongestion in admitted patients (Mullens, 2011). Congestion is a term from cardiology literature used to describe vascular congestion and the resultant third space volume shift. Several scoring systems exist and there is no consistent definition for this term.
The ADVOR trial was multi-center, double-blinded, randomized-control trial conducted at several academic centers in Belgium from 2018-2022. There, 519 patients were admitted with acute decompensated heart failure (treated as outpatients for at least one month with a least 40mg of furosemide or equivalent dose of another loop diuretic) were enrolled.
Inclusion criteria included B natriuretic peptide (BNP) > 250 pg/mL or N-terminal pro-B-type natriuretic peptide (Nt-proBNP) > 1000 pg/mL plus one clinical sign of volume overload.
All patients received intravenous loop diuretic at double their home dose initially and once per day on study day two through three.
The control group received a placebo, while the treatment group received a 500mg IV bolus of acetazolamide at randomization and daily for the next 48 hours or until complete decongestion in addition to intravenous loop diuretic.
The primary outcome was successful decongestion, assessed by a cardiologist using an unvalidated congestion score.
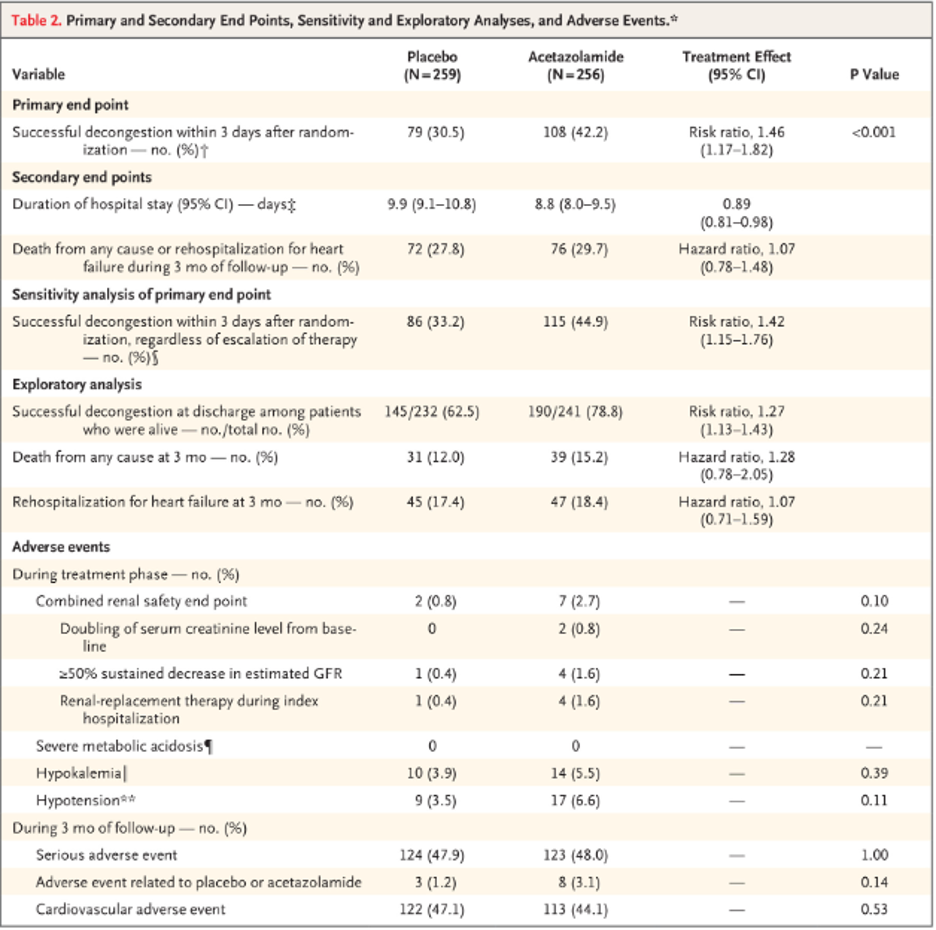
Successful decongestion was achieved in 42% of the treatment group compared to 31% in the placebo group at day 3 of hospitalization (RR 1.46 [1.17 to 1.82], P-value < 0.001). At 48 hours of hospitalization, both diuresis (4.6 L in acetazolamide group vs 4.1 L in placebo) and natriuresis (468 mmol in acetazolamide vs 369 mmol in control) trended towards improvements in the treatment group.
Several secondary endpoints were assessed, most notably length of hospital stay (9.9 days in placebo group vs 8.8 in the acetazolamide group, CI 0.89 [0.81-0.98]) and rehospitalization for heart failure (18% in the acetazolamide group vs 17 in the control group, Hazard Ratio 1.07 [0.71-1.59]). Death from any cause at 3 months was also assessed (15.2% vs 12.0%, HR 1.28 [0.78 – 2.05]).
None of the secondary outcomes reached statistical significance, although the safety endpoints do trend towards worsening kidney function (hyperkalemia, acute renal insufficiency, renal replacement therapy) kidney damage in the acetazolamide group.
Limitations
There are several limitations to this study.
The primary end point of decongestion is difficult to draw conclusions from, given it is an unvalidated score. Practice pattern differences in Belgium compared to the U.S. limit this study, as patients with pedal edema and a small pleural effusion are often discharged from the Emergency Department in the U.S. without admission. Powering future research to look at decreased length of stay or decreased mortality would increase the impact of this study.
Secondly, the homogeneity of their study population limits external validity to the more diverse population we see in the emergency department in the U.S. A letter to the editor was published in NEJM noting a significant difference in the number of patients taking Mineralocorticoid receptor antagonists (50.4% in acetazolamide vs 42.3% in control) (Culic, 2022). This difference further limits the generalizability of this study as mineralocorticoid receptor antagonists are potent diuretics and have been shown to improve outcomes in patients hospitalized with heart failure, potentially biasing the results (Culic, 2022).
CONCLUSION
The ADVOR Trial is a well-designed study that shows the addition of acetazolamide to standard of care diuresis for acute heart failure exacerbation improves congestion, diuresis, and natriuresis. It is difficult to draw useful clinical data from this study and apply it to care in Emergency Department in the U.S. While there may be some patients admitted with heart failure who benefit from the addition of acetazolamide to their diuretic therapy, especially those with hypernatremia, further research is needed to investigate the routine use of acetazolamide in the initial management of acute heart failure exacerbation.
CASE RESULT
The patient is given 40 mg of IV Furosemide. While boarding in your emergency department, he has over 1.5 L of diuresis. His oxygenation improved and he was admitted to the hospital for further management.
REFERENCES
Heidenreich PA, Albert NM, Allen LA, et. al.: Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013; 6: pp. 606.
Agarwal MA, Fonarow GC, Ziaeian B. National trends in heart failure hospitalizations and readmissions from 2010 to 2017. JAMA Cardiology. 2021; 6:952–956.
Heidenreich PA, et al.: 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022. 145. 18.
Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999; 341:709–717.
Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms.N Engl J Med. 2011; 364:11–21.
Ellison DH, Felker GM. Diuretic treatment in heart failure.N Engl J Med. 2017; 377:1964–1975.
Wilson JR, Reichek N, Dunkman WB, et al. Effect of diuresis on the performance of the failing left ventricle in man.Am J Med. 1981; 70:234–239
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599-3726.
Kassamali R, Sica DA. Acetazolamide: a forgotten diuretic agent. Cardiol Rev. 2011 Nov-Dec;19(6):276-8.
Mullens W, Troisfonatines, P, et al. Acetazolamide in Acute Decompensated Heart Failure with Volume Overload. New England Journal of Medicine. 2022; 387:1185-1195.
Vaduganthan, M, Hernandez, A, et al. SGLT2 inhibitors in patient with heart failure: a comprehensive meta-analysis of five randomized controlled trials. The Lancet. 2022. 400, 10354. 757-767.
Culic, Viktor. Acute Decompensated Heart Failure, Volume, and Acetazolamide. The New England Journal Of Medicine. 2022. 387:2485-2487.